GAMMAGARD
Reimbursement Gammagard
5/2/20051 min read
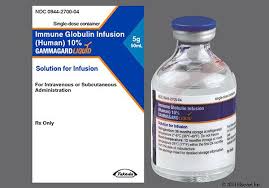
[Human Immune Globulin Infusion] GAMMAGARD LIQUID 10% is an immune globulin treatment used to treat multifocal motor neuropathy (MMN) and primary immunodeficiency (PI) that is given intravenously (IV) or subcutaneously (SC).
For proper reimbursement and compliance, accurate billing and coding are necessary. The main billing and coding rules for GAMMAGARD LIQUID are shown below:
HCPCS Codes: J1569: Intravenous injection of immune globulin (GAMMAGARD LIQUID), non-lyophilized (liquid, for example), 500 mg.
Note: The intravenous (IV) mode of administration is expressly described by this code. Providers should ask the payer for the correct HCPCS code for subcutaneous (SC) administration, as J1569 might not be applicable.
Codes for Home Infusion Therapy: S9338: Immunotherapy, home infusion therapy, administration services, professional pharmacy services, care coordination, and all required equipment and supplies (drugs and nurse visits classified separately), per diem.
Note: When billing for home infusion therapy services, healthcare practitioners should get advice from payers on proper coding.
The proper Current Procedural Terminology (CPT®) codes that specify the mode of administration (IV or SC) should be used when billing for the administration of GAMMAGARD LIQUID. To find the appropriate administration codes, providers should consult the most recent edition of the CPT® manual and payer policies.
Extra Billing Considerations: Administration Route: Verify that the HCPCS code utilized matches the administration route. J1569 is intended for intravenous administration, as said. Check with the particular payer to confirm the correct code for SC administration.
Immunoglobulin treatments are subject to prior authorization requirements under many insurance policies. Before starting treatment, make sure that all required approvals have been received.
Documentation: Keep comprehensive medical records that include the diagnosis, treatment plan, dosage, administration route, and specifics of the administration. This paperwork enables efficient claims processing and substantiates medical necessity.
